Fernando Alemanno MD
fernando@alemannobpb.it
www.alemannobpb.it
codice-fiscale: LMNFNN39M17I551W |
|
 |
|
Sonography may be useful when the subclavian artery pulse is absent;
however it can be used when all the reference points are present.
|
 |
The procedure is as follows: after having drawn the angle and its bisectings-line (or the straight line when the pulse can be felt)... |
|
 |
... we apply a linear probe to the posterior edge of the medial half of the clavicle... |
|
 |
... and slide it slowly in a lateral direction... |
|
 |
... at a certain point the subclavian artery will appear on the screen as a pulsating “black hole” and just lateral to this we can see the “circular crowns” (nervous tissue surrounded by the epinevrium) of the brachial plexus components, cut transversely by the U.S. beam. |
|
 |
Since the presence of the probe and the clavicle together hamper the insertion of the needle, according to the safe direction described in our technique... |
|
 |
...we rotate the probe about 45° degrees, in a clockwise direction on the right side and anti (counter) clockwise on the left, while observing the artery on the screen. |
|
 |
The sonographic image will essentially remain the same, but by rotating the probe we will see the bisecting-line or the straight-line needed to direct the needle, as described in our technique, and we will have enough space for its insertion “out- of- plane”. |
|
 |
To have an in-plane insertion the probe is applied on the line laterally tangent to the subclavian artery pulse or on the bisecting line of the angle if the subclavian artery pulse is absent. |
|
 |
Thus, the image shown by the ultrasound will completely differ and the elements of the brachial plexus, longitudinally cut, can be seen between the anterior and middle scalene muscles.
The arterial tube, cut along its syphone by the probe, will be seen as a hypoechogenic oblonged oval surrounded by a more or less hyperoechogenic wall, proportional to the arteriosclerosis degree. |
|
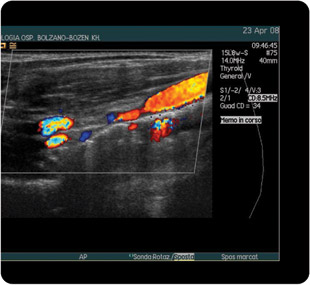 |
The same image with color-dopler effect |
|
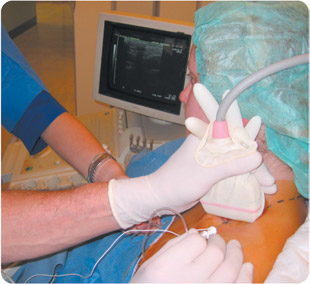 |
Here we can see the images of the combined method: NEUROSTIMULATION + U.S. GUIDE |
|
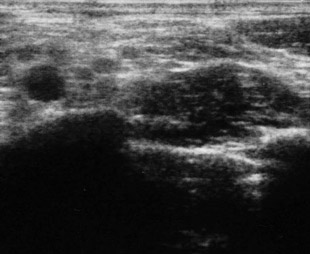 |
This picture shows the black hole of the subclavian artery and, close to it, the brachial plexus components transversely cut. |
|
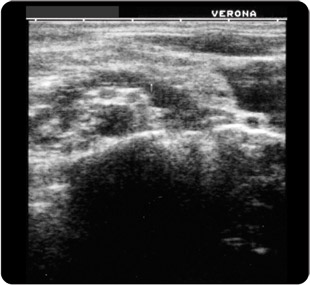 |
After having evoked the required twitch with a 0.3 mA current, we may notice the typical expansion of the anaesthetic fluid within the neurovascular bundle covered by a cloak, by a mantel of anesthetic solution. |
|
AND NOW SOME INTERESTING OPINIONS
|
 |
M.J. Fredickson MD
From the Department of Anesthesiology, Faculty of Medical and Health Sciences, the University of Auckland, New Zealand.
This sentence makes us wonder if with U.S. there are sometimes problems. The images are not always clear enough, also in the hands of an expert. |
|
 |
Brian Sites MD
From the Departments of Anesthesiology and Orthopedic Surgery, Dartmounth Medical School, Lebanon New Hampshire.
The
paper is one of the clearest theoretical pubblications about U.S. management |
|
 |
Alain Borgeat, Professor and Chief-of-staff, Department of Anesthesia, Balgrist University Hospital, Zurich, Switzerland |
|
 |
S 43 Admir Hadzic, Professor of Clinical Anesthesiology Columbia University of Physicians and Surgeons, Director New York School of Regional Anesthesia.
Author of the most complete and thorough textbook of Regional Anesthesia, published in the 2007. |
|
 |
|
 |
|
To sum up:
We have not to work in function of the probe, but the probe must work in function of the applied technique, checking the right direction of the needle and the expansion of the anaesthetic fluid when the required twitch is obtained.
Ultrasound gives us anatomical images and dynamic effects which arouse enthusiasm, but
we must not think to have found the solution to every problem.
THE LAST ARTICLE
The Echo-Guided Middle Interscalene Block,
ten years later
Alemanno F, Arnone S, Bronzini N, Cosio R.
Department of Anesthesia and Intensive Care, Istituto Clinico S. Anna, Brescia – Italy
Corresponding author:
Fernando Alemanno; e-mail: fernando@alemannobpb.it
Abstract
The authors, after having described the evolution of the Middle Interscalene Block (MIB), delineate the ultrasound-guided technique. MIB had obtained a success rate of 96.2% with only the use of the electroneurostimulation (ENS). In the last three years, with both the techniques together, in a population of 1227 patients scheduled for rotator cuff repair, the 100% success rate has been reached.
Key words: US-guided brachial plexus block – Interscalene Block – Brachial plexus anesthesia
Background
The Middle Interscalene Block (MIB) was ideated at the beginning of the nineties (1) to avoid pneumothorax, possible with supraclavicular techniques like Kulenkampff’s, and the danger of subarachnoidal or intravertebral artery injection possible with other techniques which are too near to the cervical column. At that time we used paresthesia to understand if we had come into contact with the nervous structure, following Daniel C. Moore’s aphorism “no paresthesia, no anesthesia”(2). At the end of the last century the technique getting the aid of electroneurostimulation (ENS) gained comfort and safety. In the November-December 2006 issue of Regional Anesthesia and Pain Medicine, “The Middle Interscalene Block: Cadaver Study and Clinical Assessment” was published (3). The article reported an important anatomic study verifying the safety of the insertion line of the needle. The article was preceded in the same issue by a Harrop-Griffiths and Denny’s editorial that rightly put the question if in the ultrasound age does a need exist for new blocks? (4) Stimulated by the constructive criticism we began to apply the ultra-sound support to the Middle Interscalene Block (MIB), a technique already having a success rate of 96.2%.
Method
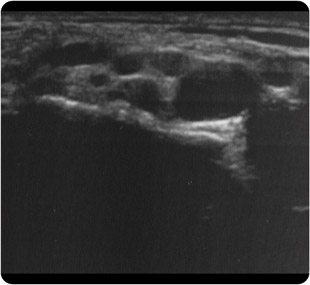
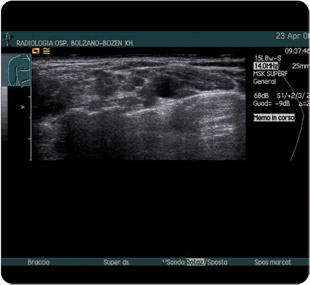
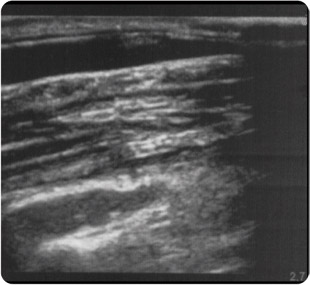
The aim of the base-technique is to cannulate the neurovascular bundle inserting the needle 1-2 cm posteriorly the midpoint of the clavicle along the straight line that from the midpoint is lateral-posteriorly tangent to the subclavian artery pulse. The needle direction must be parallel to the transverse plain of C7, identified by the C7 spinous process, the superior midpoint of the clavicle and the superior point of the sterno-clavicular joint (three points identify a plane). If the subclavian artery pulse is not present, joining the midpoint of the clavicle to the other two we draw an angle, whose bisecting line corresponds to the brachial plexus way. With the ultrasound guide it is the same if the subclavian artery pulse is palpable or not. A linear probe is applied medially on the posterior edge of the clavicle (Fig.1); slowly sliding it laterally, the pulsing black hole of the subclavian artery will appear and laterally superiorly to it the brachial plexus (Fig.2). Of course, the clavicle and the probe hamper the insertion of the needle according to the direction before described, therefore we have to rotate the probe about 45° in a clockwise direction on the right side and counterclockwise on the left, always being careful not to lose view of the pulsing subclavian artery (Fig.3); the brachial plexus image will not substantially change: before the brachial plexus components were a little obliquely cut (like a slice of salami) now they appear transversally cut(Fig.4). The ideal straight line that leads to the brachial plexus, with the rotation of the probe, now appears free and we can insert the needle after having injected 0.5 ml of anesthetic solution for an intradermic infiltration. Obviously, the echo-guided technique is “out of plain” and we will see tissue movement under the push of the needle. After having evoked the proper twitch (deltoid, triceps or biceps muscle), we may observe the anesthetic spread into the brachial plexus bundle (Fig. 5-6-7).

Fig. 1. A linear probe is applied medially, on the posterior edge of the clavicle
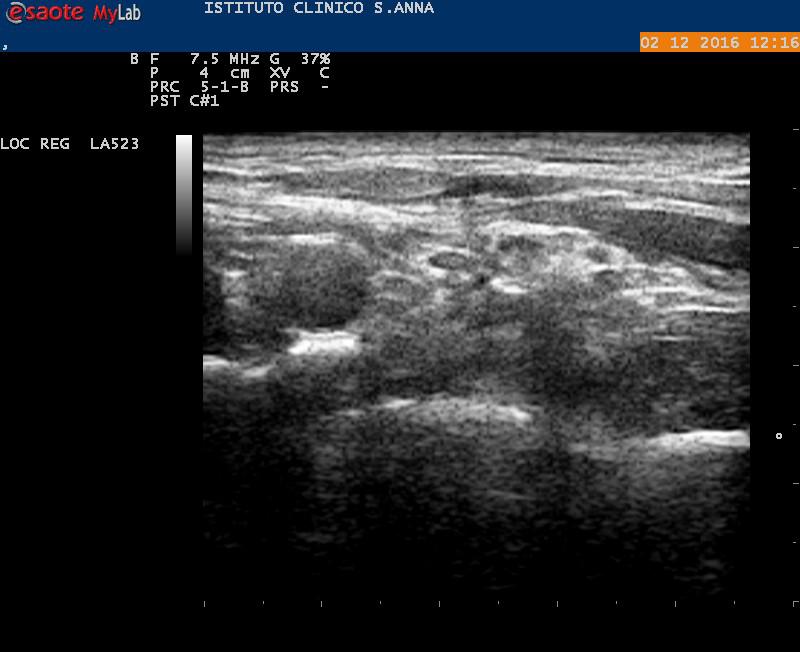
Fig. 2. View of the neurovascular bundle with the probe applied behind the clavicle and parallel to it. The brachial plexus components are obliquely cut (like a slice of salami).
 Fig. 3. The probe is rotated about 45°
Fig. 3. The probe is rotated about 45°
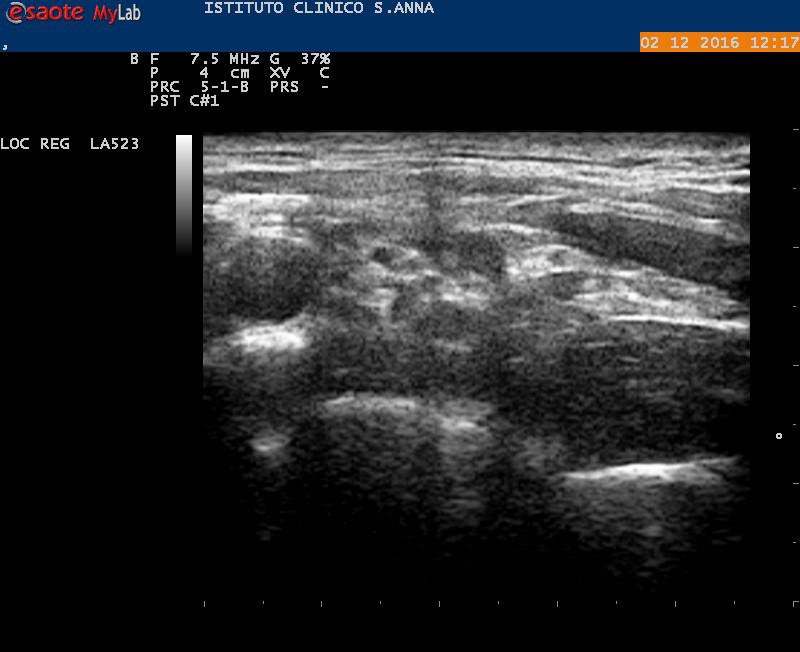
Fig. 4. After having rotated the probe, the brachial plexus image will not substantially change; except that the brachial plexus components appear transversally cut.
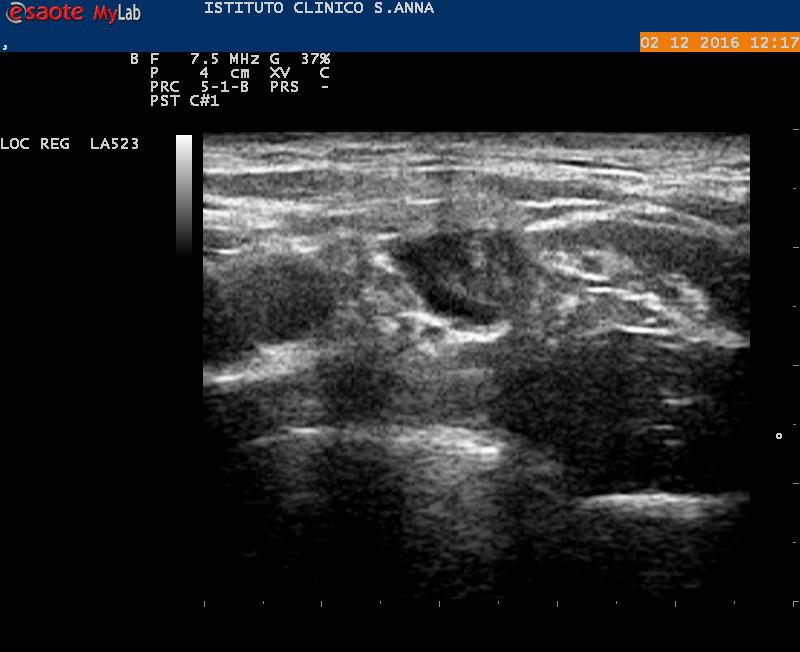
Fig.5. Spread of the first 5 ml of anesthetic solution into the brachial plexus.
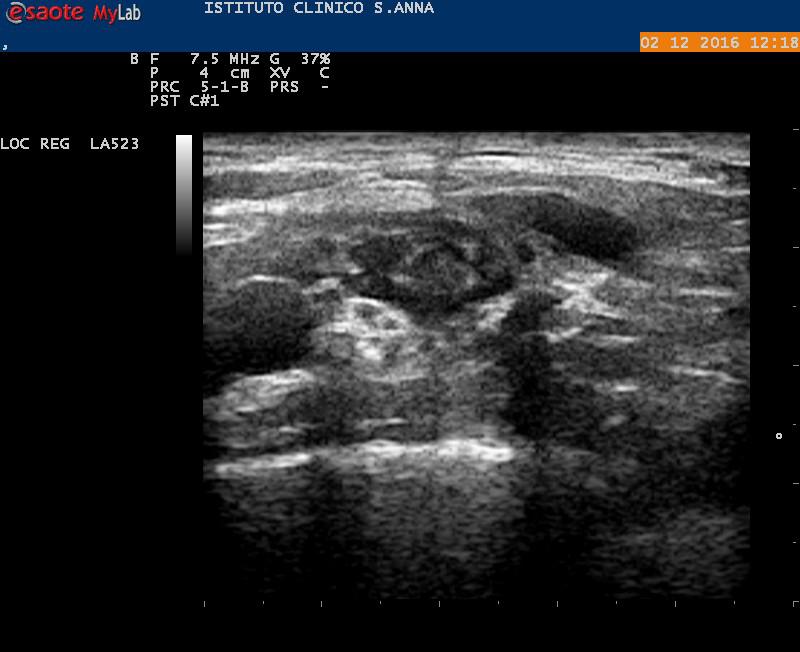
Fig. 6. Spread of the first 10 ml of anesthetic solution.
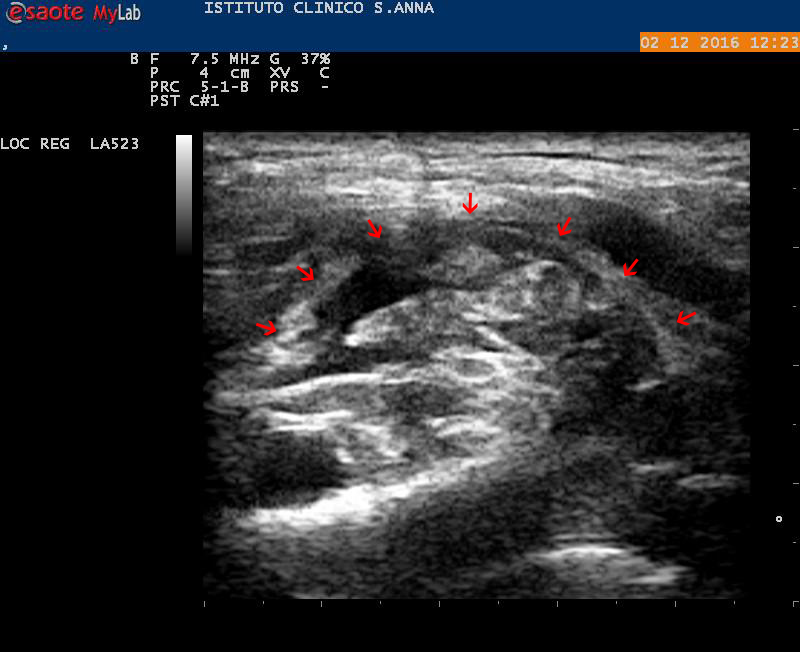
Fig 7. Now, after having injected 32 ml of local anesthetic, we can note that the brachial plexus is completely surrounded. Also evident the cervical sheath (red arrows), that wraps the neurovascular bundle.
Results
The first technique’s report about the ultrasound guided middle interscalene block was presented as a poster at the 2008 ESRA Congress in Genoa (5). Until 2006, with the use of the ENS only, on a population of more than 700 controlled patients, we obtained a success rate of 96.2% (3). The technique was summarily reported in the book “L’Anestesia Dell’Arto Superiore” (6) in the Italian language and in the English version “Anesthesia of the Upper Limb” (7). After having refined the U.S. guided MIB, we have ascertained that in the last four years, for the period 2013 to 2016, applying the technique to 1227 patients, scheduled for arthroscopic cuff repair, we reached a 100% success rate, without any complication.
Conclusive considerations
To the Middle Interscalene Block may be attributed the exclusive use of “out of plain” modality. As a matter of fact, the “in-plane” modality is practicable with difficulty, because the concavity of the supraclavicular region badly suits a linear probe lined up along the plexus direction. But, the poor vision of needle progression, limited to the tissue’s movements, is counterbalanced by the insertion line’s safety, which has been anatomically proved (3). The US spread image of local anesthetic (Fig. 5), injected after ENS, further contributes to controlling the right position of the needle. To sum up, U.S. application to MIB has given further safety and success rate to a technique that already proved to be safe for the anatomic plane followed by the needle and that, with only the aid of ENS, gave a high rate of success (96.2%). The echographic implementation has obtained 100% success. Therefore, we agree with Admir Hadzic: “…ultrasound and nerve stimulation are complementary and not mutually exclusive monitoring technologies” (8).
Bibliography
1) Alemanno F. Un nuovo approccio al plesso brachiale. Minerva Anestesiol, 1992; 58 (6): 403-406.
2) Moore D C. Regional block. A handbook for use in the clinical practice of medicine and surgery. Charles C. Thomas Publisher, Springfield, Ilinois, U.S.A. 1965.
3) Alemanno F, Capozzoli G, Egarter-Vigl E, Gottin L, Bartoloni A. The middle interscalene block: cadaver study and clinical assessment. Reg Anesth Pain Med. 2006; 3: 563-568.
4) Harrop-Griffiths AW, Denny NM. Eponimity and the Age of Ultrasound: how should the new blocks be introduced into the clinical practice? Reg Anesth Pain Med. 2006; 3: 492-495
5) Alemanno F. The Ultrasound Guided Middle Interscalene Block. Reg Anesth Pain Med, 2008 ; Volume 33 (5): 117. Peripheral nerve block: Poster.
6) Alemanno F, Bosco M. Barbati A. L’Anestesia dell’Arto Superiore – 100 anni dopo (1911-2011). Verduci Editore, Roma 2011.
7) Alemanno F, Bosco M. Barbati A. Anesthesia of the Upper Limb – A state of the art guide. Springer Verlag, Milan Heidelberg New York Dordrecht London, 2014.
8) Hadzic A. Nerve Stimulation Shouldbe used in Conjunction With Ultrasound-Guided NerveBlocks. ASRA NEWS, November 2007,
pp 7-9
|
|
 |
|